In a new study entitled “Mutation in MRPS34 Compromises Protein Synthesis and Causes Mitochondrial Dysfunction,” researchers discovered a mutation in a mitochondrial ribosome that induces mitochondria dysfunction leading to heart hypertrophy and liver steatosis in mice. The study was published in the journal PLOS Genetics.
Mitochondria are the organelles inside eukaryotic cells responsible for producing cells’ energy, and are thus vital organelles for cell’s normal function and survival. While mitochondria possess their own DNA, the mitochondria-DNA (mt-DNA), they are regulated by both mitochondrial and nuclear genome. Increasingly recognized are the so-called mitochondria diseases, which usually arise as a result of mutations occurring in nuclear genes that code for mitochondria proteins. These are characterized by mitochondrial dysfunction and therefore defective in energy production, which is a similar phenotype that characterizes several metabolic diseases.
Here, researchers were curious as to how deregulating mitochondrial gene expression and underlying processes impair mitochondria function. The team focused on the mitochondrial ribosomal protein of the small subunit 34 (MRPS34), a mitochondria-specific ribosomal protein, and studied its function in mice. To this end, the team generated a mouse with a mutation in the gene coding for MRPS34 resulting in a significant decrease in MRPS34 expression in both heart and liver. They observed that Mrps34 mutated mice exhibited reduced levels of the 12S ribosomal RNA (rRNA), hinting that MRPS34 is required for its stability. Notably, the team also observed that this mutation reduced the levels of specific mitochondrial mRNAs in the liver, but not in the heart. Therefore, Mrps34 mutation impairs mitochondria RNA metabolism in a tissue-specific manner. Since MRPS34 is a ribosomal protein (ribosomes are the locations inside the cell where protein synthesis occurs), the team determined how it affected mitochondrial protein synthesis. They observed that indeed there was an overall decrease on protein synthesis and on mitochondrial respiratory complexes in the livers on mutated mice.
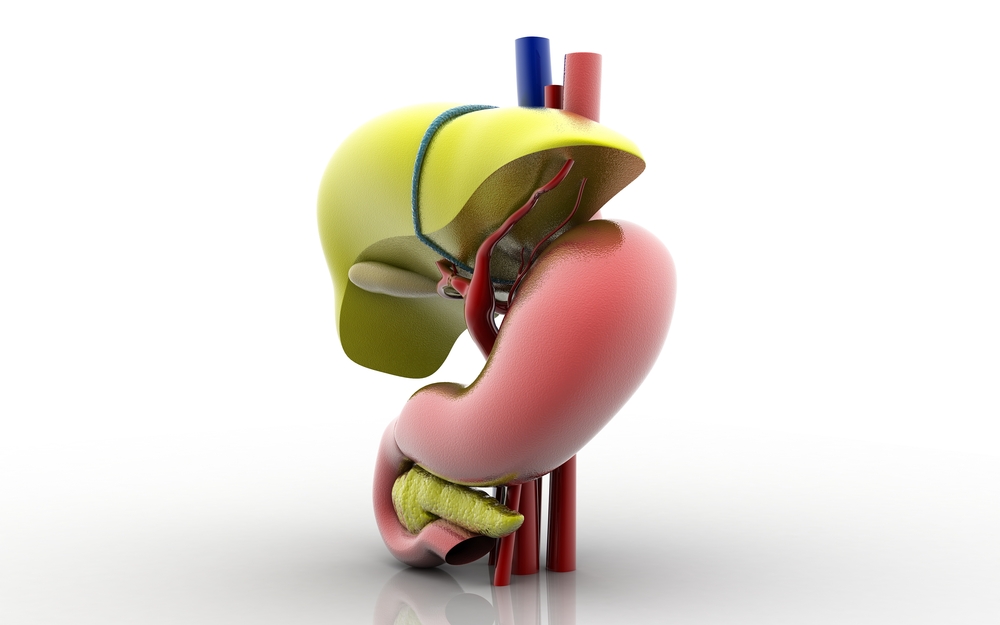
The team further analyzed both hearts and livers of mutated mice, since previous reports suggested that these type of mutations were linked to cardiomyopathy in patients. They showed that Mrps34 mutation induced heart hypertrophy and liver steatosis (this denotes the accumulation of fat in the liver) with age.
The authors noted that their results show that Mrps34 mutation causes mitochondria dysfunction, leading to heart abnormalities and progressive liver disease. This mouse model can help researchers dissect the pathogenic mechanisms of metabolic syndromes linked to mitochondria dysfunction.
Dr. Tara Richman from the Mitochondrial Medicine and Biology Laboratory at Harry Perkins Institute of Medical Research, Australia noted in a press release, “It’s been very interesting to see through our work in the laboratory that even though there may be a mutation in the mitochondria in other cells of the body, the liver is most severely affected. This may be due to the fact that proteins synthesize faster in the liver than in other organs such as the heart, so this is a big step forward in our understanding. We now have a great model for future testing of treatments for fatty liver disease.”