A long-term study led by researchers at the Johns Hopkins University School of Medicine suggested a link between elevated coronary artery calcium (CAC) scores and the risk of developing not only cardiovascular disease but also cancer, chronic kidney disease (CKD), and chronic obstructive pulmonary disease (COPD).
The study, “The Association of Coronary Artery Calcium With Noncardiovascular Disease : The Multi-Ethnic Study of Atherosclerosis” was published in the journal JACC: Cardiovascular Imaging.
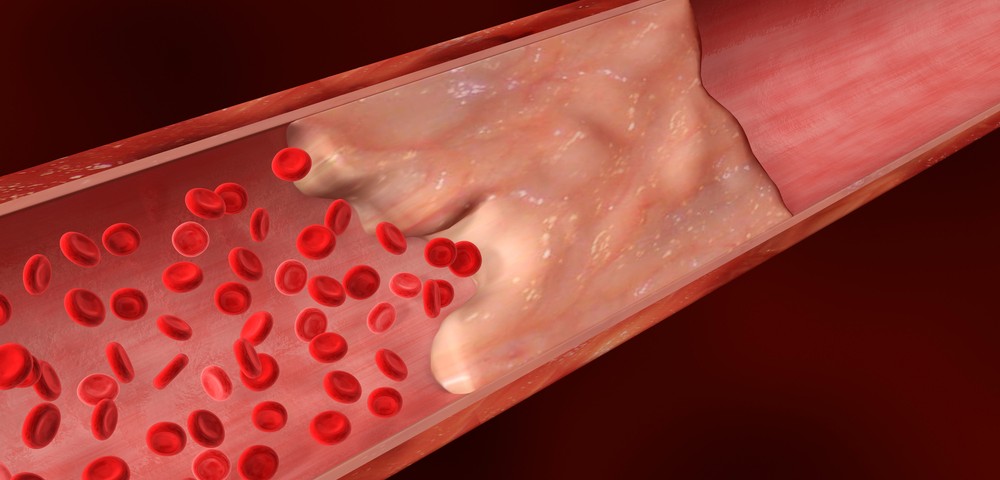
According to the U.S. Centers for Disease Control and Prevention, coronary and vascular disease, cancer, and kidney and lung diseases are leading causes of death in the United States. CAC deposits, or plaque, are a well-known predictor of heart and vascular disease, with modest scores translating into a lower risk and scores above 400 indicating a substantial risk. Calcium deposits in the arteries can be estimated using heart CT scans.
“Plaque in the arteries is the result of cumulative damage and inflammation, and vulnerability to injury and chronic inflammation likely contributes to diseases like cancer, kidney and lung diseases, as well as cardiovascular disease. So it makes sense that the coronary calcium score — a measure of arterial aging — is predictive of noncardiovascular diseases too, “Michael Blaha, MD, MPH, director of clinical research for the Ciccarone Center for the Prevention of Heart Disease and assistant professor of medicine at the Johns Hopkins University School of Medicine, said in a press release. “The reason the coronary calcium score may work so well at identifying vulnerability to a variety of chronic diseases is because it’s a direct measurement of the cumulative effect of all risk factors, rather than a consideration of a single risk factor, like obesity, smoking or high blood pressure.”
The study included 6,814 participants, ages 45 to 84, of various ethnic backgrounds: white, African-American, Hispanic, and Chinese. During initial heart CT scans, participants had no noncardiovascular disease and no evidence of CAC. Follow-up visits of at least once a year for 10 years were conducted to screen for changes.
After 10 years, a total of 1,238 participants were diagnosed with noncardiovascular diseases: various types of cancer (prostate, lung, gastrointestinal/colon, breast, skin, and blood/uterine/ovarian), kidney disease, pneumonia, blood clots, lung disease, hip fractures, and dementia. When data from participants with and without CAC were compared, results revealed that those with CAC over 400 were more than three times at risk of developing noncardiovascular disease than those with no CAC score (36.9 percent versus 11 percent), including cancer (53 percent greater risk), kidney disease (70 percent) and COPD (63 percent). Dementia and hip fracture, however, were marginally associated with CAC scores for reasons that the researchers related to the low number of participants diagnosed with these diseases. Blood clots and pneumonia were found to have no association with CAC scores.
“Participants with elevated CAC were at increased risk of cancer, CKD, COPD, and hip fractures. Those with CAC = 0 are less likely to develop common age-related comorbid conditions, and represent a unique population of ‘healthy agers,’” the authors concluded.