Lack of vitamin D in patients with chronic kidney disease might contribute to problems with access to the blood vessels needed for dialysis, increasing the risk of worse outcomes, but more evidence is needed, according to new research from Italy.
The report, “Role of Vitamin D in Vascular Complications and Vascular Access Outcome in Patients with Chronic Kidney Disease,” published in the journal Current Medicinal Chemistry, examined the evidence supporting the role of vitamin D in this process, concluding that more studies, involving larger sets of patients, are still necessary.
Low vitamin D levels are known to lead to the development of secondary hyperparathyroidism and contribute to other complications linked to excessive inflammation and oxidative stress in chronic kidney disease patients, but studies have also indicated that it might impact hemodialysis outcomes.
A common way to access blood vessels for hemodialysis in chronic kidney disease patients is to create an arteriovenous fistula, directly linking an artery to a vein. Keeping the access open is not a straightforward process, however, and is linked to complications and failure.
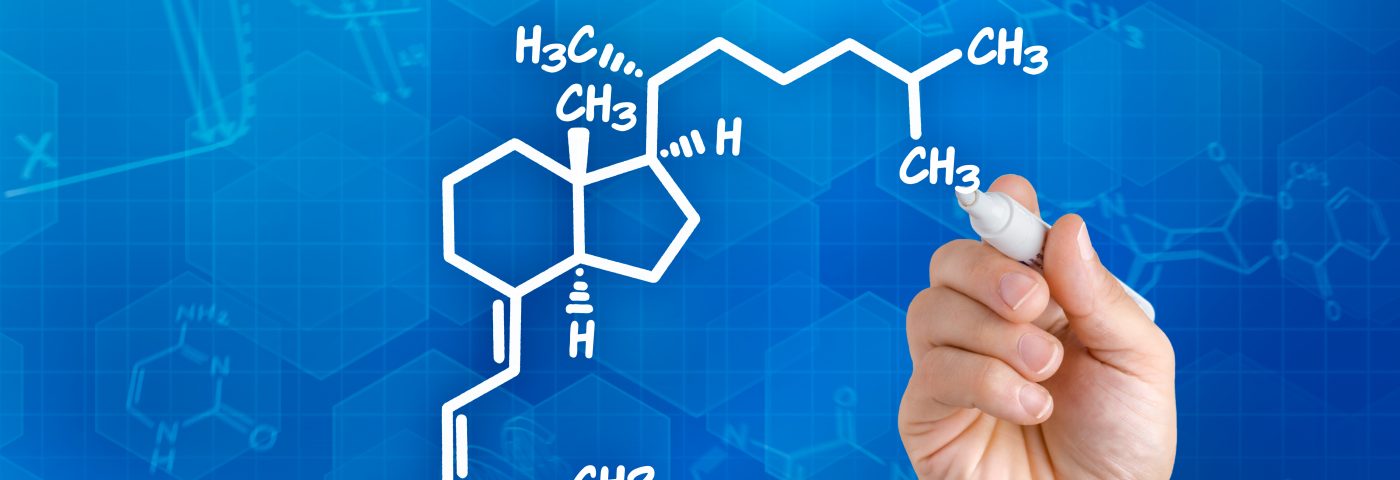
Recent research has suggested that vitamin D might be involved in blood vessel remodeling, and might contribute to the failure of dialysis access points. An activated version of the vitamin is produced by endothelial cells lining the blood vessels, which also express receptors for vitamin D.
Studies have also suggested that activation of these receptors are involved in triggering changes in the metabolic activity of these cells, that in turn may contribute to remodeling processes.
But vitamin D can act on blood vessels through several mechanisms. For example, scientists have shown that it can activate the renin-angiotensin-aldosterone system, commonly called RAAS, a hormone system that controls blood pressure. When patients are treated with drugs blocking this system, a compensatory increase in the hormone renin often results. Studies in experimental animals show that vitamin D can blunt this increase.
Other studies show that vitamin D reduces the numbers of another receptor involved in this system, called angiotensin 2 receptor. By affecting this receptor – also present on endothelial cells – research suggests that the vitamin can mediate a cascade of events that result in the production of vasodilators, such as nitric oxide.
This essential vitamin also affects the rate at which cells divide, and controls pathways preventing cell death. Mutations in the vitamin D receptor gene have also been linked to heart disorders and chronic kidney disease.
Recently, two retrospective studies and one randomized prospective clinical trial directly investigated whether vitamin D could impact the success of vascular access, but reached different conclusions. Additional studies are necessary involving larger number of patients to better understand the potential relationship between vitamin D and vascular access outcomes.